Institutional Claims FAQs
How do I access the Institutional Claims APIs?
The Institutional Claims APIs enables healthcare providers to submit institutional healthcare claims for a service or encounter.
What information goes in the API Request header?
Please see example in API Request Header.
How do I check the Operating Status of the API?
/institutionalclaims/v1/healthcheck endpoint checks the operating status of the Institutional Claims API engine. See example in API Health Check.
Do you have a sandbox that I can test with before signing a contract?
Yes, we do, see Sandbox FAQs and API environments.
What does a typical Institutional Claims API request look like?
The Institutional Claims Submission API uses the POST request. Responses to our Medical Network APIs can be lengthy due to the many data points that a payer or trading partner provides in the query response. This is especially true since institutional claims can have hundreds of line items in the claimInformation object (Loop 2300 in the EDI spec), each of which reflects payer decisions on payment.
Our APIs translate back and forth between JSON and X12 EDI when the information departs into and returns from the medical network. All fields and JSON objects conform to the EDI 837i transaction standard.
NOTE
See example in the API Examples section on the left panel in the developer portal.
Institutional claims v1 request example
This example is brief compared to what can apply in a real-world transaction: Institutional Claims Request & Response.
How to handle multiple authorization numbers per claim?
Please see example in Handle Multiple Authorization Numbers per Claim.
What does a typical Institutional Claims API response look like?
Please see example in Institutional Claims Request & Response.
What do Institutional Claims error responses look like?
Please see example in Institutional Claims Error Response.
If something is wrong with the syntax of the data, you may get a response from our validation endpoint. See example in Institutional Claims Syntax Error Response.
How do Institutional Claims work for Medicare?
Medicare payers accept claims only for subscribers. If you want to submit a dependent claim with a Medicare payer, submit the dependent as a subscriber in the claim request. For more information, see Institutional Claims for Medicare.
What is the difference between an Institutional claim and a Professional claim?
- Professional billing typically uses the 837p transaction (or the CMS-1500 form in hard copy)
- Institutional billings use the 837i transaction
We support both types of electronic claims and transactions. Institutional billing also sometimes encompasses collections while Professional Claims and billing typically do not.
Professional billing controls the billing of claims generated for work performed by physicians, suppliers, and other non-institutional providers for both outpatient and inpatient services. One commonality: our APIs help support and automate insurance coding for both Institutional and Professional claims.
What is the claimReference field in the Submission response?
The claimReference field is an object containing the list of identifiers that you can use to track an Institutional Claim. Please see example in ClaimReference Field in Submission Response.
claimReference object fields
Please claimReference objet fields in ClaimReference Field in Submission Response.
How to create EDI 837p 5010 claim for a client that has both Primary and Secondary insurances?
Please see example in Primary and Secondary Insurances-Create EDI 837p 5010 Claim for a Client.
If the Primary claims are sent electronically, will the Secondary/Tertiary claims be sent electronically as well all the time?
For the secondary claim to be paid electronically, the primary payer must accept secondary claim. Please see example in Primary, Secondary, and Tertiary Claims.
What is a tradingPartnerServiceId?
This value is also known as the payer ID (a number you will find on your insurance card).
- The request for Eligibility needs the
tradingpartnerServiceIDto be the Realtime Payer ID found on the ConnectCenter Payer List (see the following snapshot). - While the request for Claims needs the
tradingPartnerServiceIDto be the CPID found on the ConnectCenter (see the following snapshot).
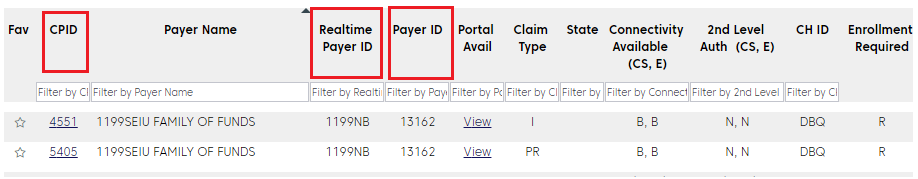
The column on Payer Tools >> Payer Search shows the Payer ID (one that is on your insurance card), which is a 5-digit value, such as "aetna" or "87226" for United Healthcare. Enter this value in the the search box to 'cross-walk' and find the Realtime Payer ID or CPID. In essence, all the three values pertain to which payer the request is sent to.
Can we electronically bill Worker's Compensation?
Our APIs can transmit accident and worker's compensation claims.
A provider has two different teams; one enters the claim and the other verifies and submits it. Before submitting, can they enter the claim, save it and have it released when ready?
Our APIs do not have a caching/drafting feature. Customers can develop and automate this feature. Customers should hold the claims at their end, and programmatically set up a console to separate working on claims from submitting them.
For EDI claims, where can I put the session times in Loop 2400 for each individual line in the claim request when using the claims API?
In the developers portal's JSON-to-EDI mapping, scroll down to Loop 2400 to view different SV segments.
How to avoid the error "OTHER PAYER PRIMARY ID# IS MISSING OR INVALID" when the other payer doesn't have a payer ID and for which the claims are set up to be sent by paper?
Please error message description in Other Payer Primary ID is Missing or Invalid.
What is the Claim submission Flow in Change Healthcare?
Please see steps in Claim Submission Workflow.
Does Change Healthcare support appeals for denials? Are there any APIs through which these appeals can be submitted?
Please see example in Corrected Claim in Appeals and Denials.
How do you re-submit a claim that was denied – Appeal & Denial
Please see example in Corrected Claim in Appeals and Denials.
Can we submit multiple claims at once, in batches?
We do offer batch submissions through SFTP only, our current API does not allow for batch submissions. These would have to be 5010-compliant EDI files. Please reach out to your sales representative to discuss pricing options for SFTP submissions.
When a claim is submitted via the API, the API returns a change healthcare claim ID. What API can I use to fetch the payer's claim number before we receive the ERA, ideally the next day after the claim is submitted successfully?
The payer-assigned claim ID would be returned through the SF and SD reports we provide through the responses and reports API. Additionally, you may be able to check the provider portal for the payer for this information.
Can you provide the source to obtain the master list related to CMS1500/UB04 Claims forms?
Optum does not have a master list of information.
- 1500 is a medical claim (Professional) – When paper is sent, this form is used for Medical claims
- UB04 is hospital claim (Institutional) – For Hospital
- 837P is a 1500 Medical Claims
- 837I is a UB04 Hospital claims
The information is common across the medical industry and there are many crosswalks or sites you can find that map the paper claim locations to a 837.
Is the usageIndicator field something that is respected by the clearinghouse and/or payers? Is submitting real data with a "T" usageIndicator value a valid way to test production data without actually submitting it for processing? How is this field interpreted?
Please see example in Test Production Data without Submitting for Processing.
Can you provide example/sample data and best testing approach to test rejected/denied claims?
Testing claims in the sandbox is limited to the predefined data values but in production. Please see example in Test Rejected/Denied Claim.
EDI NM103 1000b organization name could be either the insurance company payer or a clearinghouse, should the organization name here be the insurance payer?
Correct, this field can typically contain either the clearinghouse or payer name. We advise you send the payer name when available. Additionally, if a payer were to require specific information be present, we would make any necessary adjustments prior to submission.
How to include condition codes to the claim information?
Please see example in Use Conditional Codes in Institutional Claims.
Related Topics
Updated about 2 months ago