Quick Start
Refer to the Educational and Practical Guide for Eligibility APIs and the workflows that surround it to help you if are having trouble with the selected API and its associated workflows.
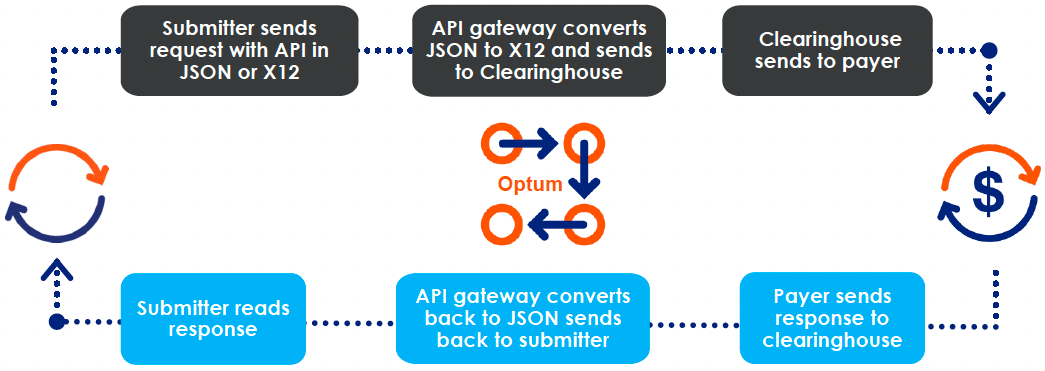
Data Flow Process
First-time users
What kind of resources do you offer in your API documentation?
In addition to resource in this developer portal, in our Getting Started guide section, you will find:
- Required fields
- Format of the returned response
- Error formats
- Examples
You can also download:
- OpenAPI specification — Every API getting started section provides links to download the file in a JSON format, which generates our documentation for developers to use.
- API Collection — For use in the Postman application; this collection allows users to call and test the APIs.
Our FAQ and API examples are periodically updated with new information. For any unanswered questions, please post them in the developer community, and we will provide suitable answers.
Explore our products
- Visit our Marketplace to explore our products.
- Based on your business type, select the product of your choice.
Create a sandbox
- Create a sandbox account without any financial obligations.
- Generate a Bearer token (authorization token).
- Try our APIs using Try It interface or using postman collection using the predefined fields and values.
IMPORTANT
The sandbox returns a canned response based on the received data. There is no validation check or confirmation of specifically required information. These checks would only occur in the production environment. You would need to manually review the companion guides offered by the specific payers to confirm what is required for each.
Explore how the JSON-to-EDI mapping works.
After you have tested and selected the product for your business type, you are ready for transiting to production environment.
Contract for production environment
Contract with us and procure your production credentials from your Optum (formerly, Change Healthcare) representative.
TIPS
- Use the quick reference list (highlighted in a purple arrow below) link in the developer portal to search for specific information that you are looking for.
- Use the left navigation (indicated by the red arrow below) for topic-wise help covered in this developer portal. Scroll down to view all of the product documentation.
Or
Click one of the product blocks (indicated by the yellow arrow below).
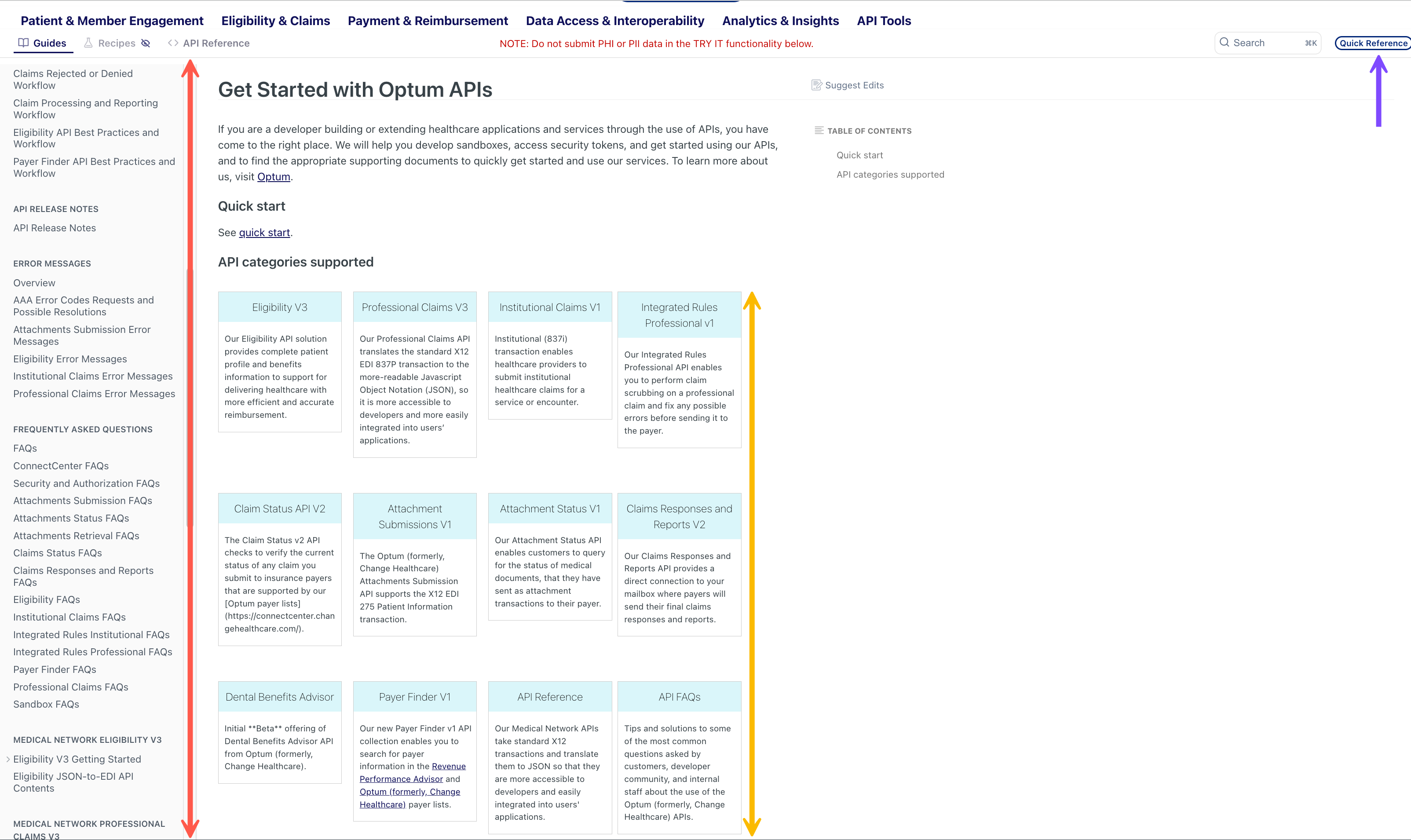
Dev Portal Getting Started
Browse by product
The Attachment Submissions v1 API allows clients to submit claim attachments and query their status. Attachment submissions take two forms: Solicited and Unsolicited. Solicited claims usually are sent by payers to providers requesting documentation for a claim. The API supports the X12 EDI 275 Patient Information transaction. It translates this standard to JSON, so it is more accessible to developers for integration into users’ applications. 📖 API Guide ✍️ API Reference |
| The Attachment Status v1 API enables customers to query for the status of claim attachment transactions (typically sending of medical information attachments) submitted to their payer. The API takes the transaction details and returns status information in a format that is understandable to the customer. 📖 API Guide ✍️ API Reference |
The Attachment Retrieval v1 API lets you search and download claim attachment documents for payers. It has search options based on date range, claim number, memberId, patient first name, and last name. This API supports legacy Change Healthcare (formerly Emdeon) network connections. For a full list of Legacy RelayHealth network connections, please reference ConnectCenter. 📖 API Guide ✍️ API Reference |
The claim submitter uses a Claim Status v2 API request to inquire about the status of a previously submitted claim. If the claim is finalized, the response provides the disposition of the claim (for example, Paid, or Denied). For Denied or Rejected outcomes, the response includes the reasons for the denial or rejection. The payer returns the response, as an X12 EDI 277 transaction, which is translated back to JSON by the API gateway. It translates this standard to JSON for developer accessibility and integration into users’ applications. 📖 API Guide ✍️ API Reference |
The Claims Responses and Reports v2 API provides a direct connection to your mailbox where payers will send their responses and reports to your claims. Retrieve valuable claim responses and reports from payers. 📖 API Guide ✍️ API References |
The Eligibility v3 API provides complete patient profile and benefits information to support healthcare delivery and more-efficient and accurate reimbursement. Providers get better front-end information to improve claiming processes and reimbursement rates. For payers, claims spend less time in pending status and a fewer rejected and reworked claims. It makes this popular EDI transaction set more accessible to developers and users’ applications. The API uses the standard X12 EDI 270 eligibility transaction, and formats it in JSON for an HTTP request. We manage the X12 standards in the background, and give you efficient access to medical subscriber or dependent plan membership, copays, coinsurances, deductibles, and more in an easy-to-use, human-readable format. 📖 API Guide ✍️ API Reference |
The Institutional Claims v1 API enables healthcare providers to submit institutional healthcare claims for a service or an encounter. A healthcare claim includes patient information, related diagnoses, procedures performed or services provided, and any related charges. This product allows for significant savings in time and a higher propensity for acceptance on the first submission. 📖 API Guide ✍️ API Reference |
The Integrated Rules Institutional API enables you to perform claim scrubbing. This allows you to fix any possible errors before sending the Institutional Claim to the payer. 📖 API Guide ✍️ API Reference |
The Integrated Rules Professional API v1 enables you to perform claim scrubbing and fix any possible errors before sending the professional claim to the payer. Using our Integrated Rules Knowledge Packs, our representatives can tailor your professional claims error checks and validations to the needs of your medical team. 📖 API Guide ✍️ API Reference |
Professional (837P) transaction allows physicians and other medical service providers to submit healthcare claims for a medical service or encounter. The Professional Claims API takes the standard established in the X12 EDI 837P transaction and translates this standard to JSON so it is more accessible to developers and easily integrated into users’ applications. 📖 API Guide ✍️ API Reference |
| 🟢 Payer Finder The Payer Finder v1 API consolidates our payer lists within Optum. This API programmatically exposes our payer lists within your applications (apps). The API searches and filters through your entire clearinghouse for information in your payer database for key pieces of information. You can find methods to list and search all the payer lists and methods that list unique fields within our payer data to help you find your required payer. 📖 API Guide ✍️ API Reference |
| 🟤 Dental Benefits Advisor An alternative to traditional Eligibility & Benefit Inquiry & Response, enables dental providers to confidently deliver the most accurate payment plan to patients based on their eligibility. For any questions, contact Dental Product Services. 📖 API Guide ✍️ API Reference |
Support
NEED HELP?
If you have a specific question and need a separate call:
- send us a message Here
or- for other modes of communication, review our support and escalation guide
or- ask a question in the interactive developer community
Resources
📹 Developer tutorials
🏢 Office hours support sessions
Related Topics
- Get Started with Optum APIs
- Eligibility API Best Practices & Workflow
- API Environments
- API URLs and Endpoints
- Visit our interactive developer community and sign up to access several learning resources.
- Attend our office hours sessions.
Updated 18 days ago