Primary, Secondary, and Tertiary Claims
Primary and secondary claims must be sent separately. Once the primary payer sends a remit on the claim, you can file a claim to the secondary payer.
For the secondary claim to be paid electronically, the payer must accept secondary claims.
You can verify that through ConnectCenter >> Payer Tools >> Payer Search. Those that have the green check mark under the column labeled '2nd CL', indicate that they accept them. The PayerFinder API indicates Y or N.
The primary claim information goes in otherPayerName, otherSubscriberInfomation, and the active payer details are submitted as normal. We do not have any documentation on what is required for secondary claims as this would be billing-specific and situational information.
For the secondary claim to be paid electronically, the primary payer must accept secondary claim.
NOTE
These payers can be reviewed in the [Payer Finder tool](https://payerfinder.changehealthcare.com/npd or https://payerfinder.changehealthcare.com/cap).
The ‘Accepts Secondary’ column is not automatically displayed.
- Click the gear icon (highlighted below) at the top-right of the list.
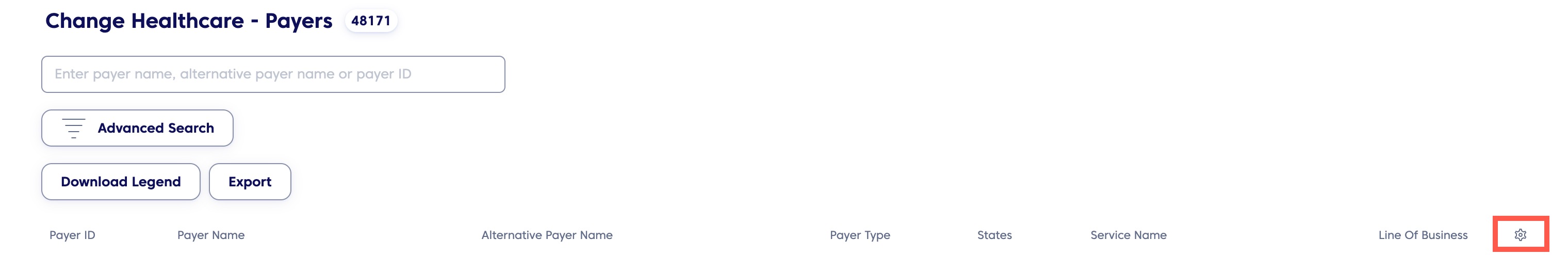
Payer Finder Tool
- From the menu that shows, select the Accepts Secondary checkbox.
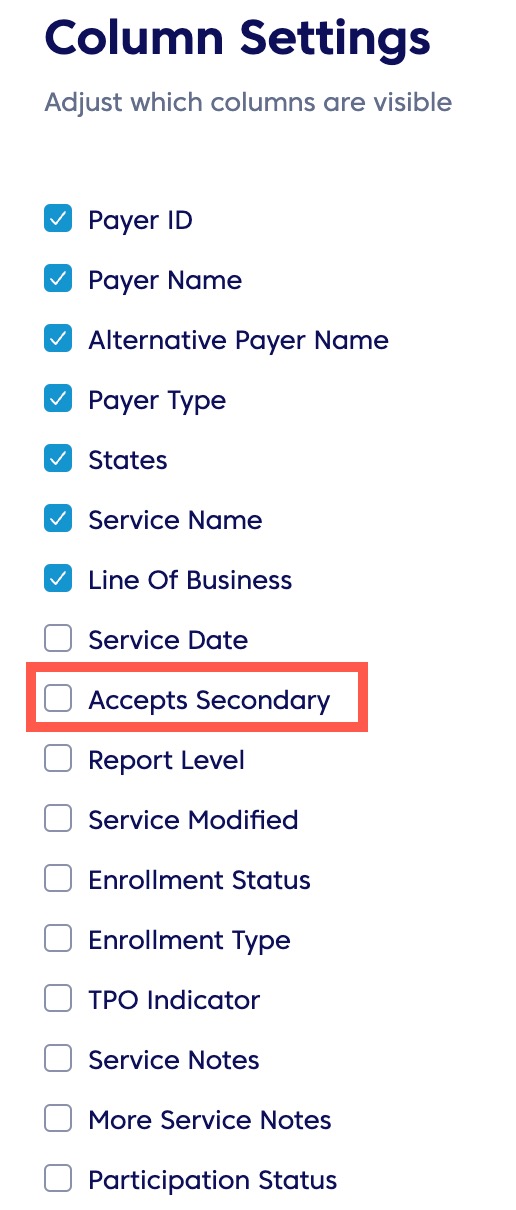
Column Settings
- Save your settings.
This will display an additional column. Those with a ‘Y’ designation, accept secondary claims.
However, the secondary payer must also process claims electronically and the appropriate payer ID must be included within the claim for the process to be fully electronic.
Updated 2 months ago